After successful periodontal treatment, many Arlington patients regain healthier gums and renewed confidence in their smiles. Osseous surgery (also called flap surgery or pocket reduction) is an advanced gum procedure used to treat serious gum disease. It is performed when deep periodontal “pockets” around the teeth remain after non-surgical treatments, making them impossible to clean with brushing or scaling. In this procedure, a periodontist or dentist gently folds back the gums, removes the diseased tissue and bacteria from the tooth roots, and reshapes the damaged bone. Smoothing the bone and reattaching the gums helps eliminate unhealthy pockets and protect the teeth. Periodontal disease is very common – over 42% of U.S. adults over age 30 have some form of it – so experienced care by trusted Arlington dentists is crucial for saving teeth and restoring oral health.
What Is Osseous (Pocket Reduction) Surgery?
Osseous surgery is a type of periodontal (gum) surgery aimed at treating moderate-to-severe gum disease by eliminating deep gum pockets and reshaping the supporting bone. When periodontitis progresses, gum tissue and bone are destroyed, creating pockets deeper than 5–7 mm that harbor harmful bacteria. During the surgery, the dentist makes small incisions to lift a gum flap and expose the tooth roots and underlying jawbone. All calcified plaque (tartar) and infection are then thoroughly removed from the exposed roots. Any uneven or spongy bone caused by the disease is carefully smoothed and contoured. This “recontouring” step eliminates bone defects so the gum can fit more snugly and heal tightly against the teeth. Finally, the gum tissue is repositioned and sutured back into place over the reshaped bone, creating shallower, healthier pockets that are much easier to keep clean.
In effect, osseous surgery converts problem pockets into shallow grooves. It is the most predictable way to reduce periodontal pocket depths and allow gums to reattach. According to experts, the goal is to “smooth and reshape bone that has been damaged by periodontal disease” and create a shallow pocket that makes it harder for bacteria to survive. In other words, osseous surgery goes beyond a simple deep cleaning; it surgically removes bacteria and restores bone contours so that your gums can heal properly.
When Is Osseous Surgery Needed?
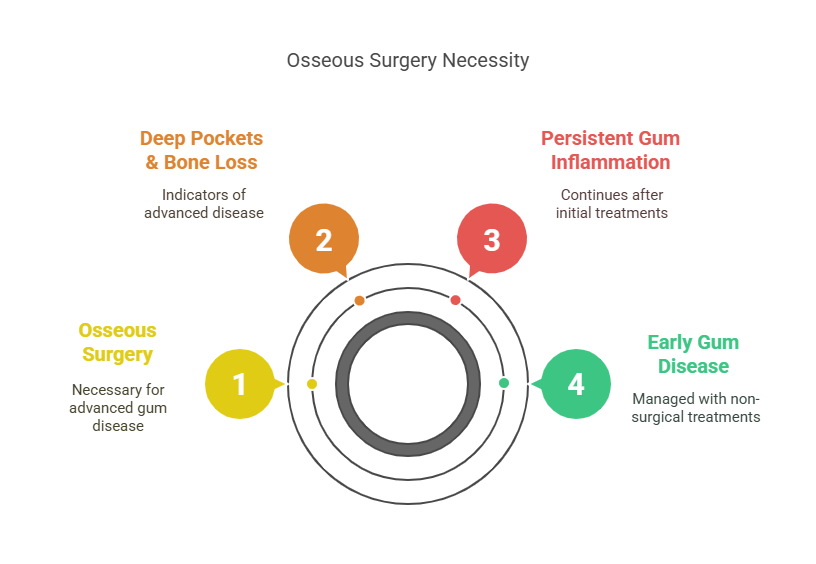
Osseous surgery is recommended when gum disease has advanced to a point that non-surgical treatments no longer work. After thorough scaling and root planing (deep cleanings), most patients with early gum disease will heal. But if X-rays or measurements show that pocket depths remain large (typically 5 mm or more) and bone loss is evident, osseous surgery becomes the next step. For example, if your dentist finds that pockets around your teeth are too deep for you to clean at home — and bacteria continue to destroy supporting bone — surgery may be advised to stop the disease cycle.
In practical terms, patients who “have pockets that are too deep to clean with daily at-home oral hygiene” are candidates for osseous surgery. This typically includes people with moderate to severe periodontitis, where gum inflammation has persisted or recurred after earlier treatments.
How Is Osseous Surgery Performed?
The osseous surgery procedure is done under local anesthesia (numbing shots), and often with options for sedation (such as oral or IV sedation) for added comfort. In Arlington, our dental specialists ensure you feel no sharp pain during the surgery. Here is a step-by-step overview of what happens during osseous (pocket reduction) surgery:
-
Anesthesia & Flap Incision: The periodontist numbs your gums with local anesthetic (like Novocain) and may offer sedation or nitrous oxide for anxiety. Once numb, small incisions are made along the gum line to gently lift back the gum tissue and create a “flap” over the affected tooth and bone.
-
Cleaning the Roots: With the roots exposed, all plaque, tartar and infected tissue are meticulously removed from the root surfaces. This feels like an intensified deep cleaning. By debriding the roots under direct vision, the dentist eliminates bacteria that a regular cleaning cannot reach.
-
Bone Reshaping (Recontouring): After cleaning, any areas of diseased or uneven bone are smoothed using dental instruments. The dentist “files down” sharp bone spurs or bone defects, restoring a more natural shape. This bone recontouring breaks up the periodontal pockets and helps eliminate spaces where bacteria can hide.
-
Bone Grafting (if needed): If significant bone loss is present, the periodontist may place bone graft material or regenerative membranes to promote new bone growth. Grafting helps restore lost bone height, which supports the final gumline and improves long-term tooth stability. Not all cases require grafts, but it is often done at the same time as osseous surgery if indicated.
-
Repositioning & Suturing: Once the cleaning and bone work are done, the gum flap is gently folded back down to its new, lower position against the reshaped bone. The dentist trims any excess gum tissue and then uses fine sutures (stitches) to secure the gums in place. Dissolvable stitches are commonly used. This final step creates a shallow, snug interface between gums and teeth.
-
Post-Op Care: After surgery, the area is often protected with gauze and ice to control bleeding and swelling. The team will give you detailed aftercare instructions, including pain management, possible antibiotics or special mouthwash, and diet recommendations.
During the entire procedure, you will feel pressure but not sharp pain. Most patients are pleasantly surprised by how routine it feels under anesthesia. Once completed, the treated site will have substantially reduced pocket depths and cleaned root surfaces.
Benefits of Osseous Surgery
Osseous surgery offers several important benefits for patients with advanced gum disease. Its primary goals and advantages include:
-
Eradicating Infection and Bacteria: The surgery allows the dentist to completely remove bacteria-laden tartar that has accumulated below the gums. By cleaning these deep pockets, osseous surgery effectively cuts off the source of the infection.
-
Reducing Periodontal Pockets: By smoothing diseased bone and reattaching gums, pocket depths are reduced. Shallow pockets are much easier to keep clean with brushing and flossing, which prevents bacteria from re-accumulating.
-
Halting Bone Loss: Active periodontal pockets cause chronic inflammation that destroys jawbone over time. Osseous surgery stops this cycle by removing the infection and reshaping the bone. This preservation of bone helps keep teeth firmly anchored.
-
Saving Natural Teeth: By controlling the disease process, surgery often prevents the need for extractions. In fact, untreated pockets can eventually lead to tooth loss; osseous surgery can be the difference between losing teeth or maintaining them long-term.
-
Improving Oral Health and Confidence: Beyond health, patients often notice that their gums bleed much less and their smile looks healthier after healing. Treating the gum disease improves gum color and contour, which enhances overall appearance and confidence.
In summary, osseous (pocket reduction) surgery tackles the destructive process of periodontal disease at its source. It is one of the most predictable and successful ways to stabilize an infected mouth.
Recovery and Aftercare
Most patients recover from osseous surgery quickly and with minimal discomfort. Initial healing of the gum tissue usually takes about 1–2 weeks. You should expect some swelling, soreness or minor bleeding for the first few days, which is normal. Swelling and pain typically peak during the first 48 hours and then gradually subside. By about 3–4 weeks most of the improvement is seen and everyday eating and brushing resumes normally.
During recovery, follow these guidelines for optimal healing:
-
Manage discomfort: Take any prescribed pain medications or use over-the-counter anti-inflammatories as directed. Use cold packs on your cheek intermittently during the first 24–48 hours to reduce swelling.
-
Oral hygiene: Keep the surgical site clean by gently rinsing with an antibacterial mouthwash or warm salt water (per your dentist’s instructions). Avoid brushing or flossing the treated area aggressively for the first week; however, continue cleaning adjacent teeth carefully.
-
Dietary precautions: Eat soft, cool foods (soups, yogurt, smoothies, mashed potatoes) for at least a few days. Avoid hard, crunchy, spicy or very hot foods that might irritate the site.
-
Follow-up visits: Plan to see your dentist 1–2 weeks after surgery to remove any non-dissolvable stitches and check healing. Extra cleanings or maintenance visits may be scheduled to ensure continued gum health.
Under normal circumstances, most patients can return to work or school within 1–2 days after surgery. Complete gum stabilization and tissue remodeling may take several months, but you will notice that your gums bleed less and look healthier soon after healing. Ultimately, following your Arlington Dental care team’s instructions exactly will make recovery smooth and comfortable.
Alternatives and Complementary Treatments
Osseous surgery is a definitive treatment for advanced gum disease, but it is part of a broader periodontal care plan. For mild to moderate gum disease, less invasive treatments are preferred. These include scaling and root planing (professional deep cleaning) and antibiotic therapies. In recent years, laser treatments (such as LANAP) have emerged that claim to treat pockets with minimal cutting. Some patients ask about these alternatives. While laser or laser-assisted treatments can help kill bacteria and may reduce discomfort, they are not suitable for every case. Many experts agree that if significant pockets persist, the traditional flap surgery (osseous surgery) remains the gold standard. It is the most predictable way to reshape bone and achieve long-term pocket reduction.
In some cases, osseous surgery is combined with guided tissue regeneration (using membranes) or bone grafting to further enhance results, especially before placing dental implants. Arlington Dental will recommend the best approach based on your specific condition. For more information about gum disease and surgical treatment options, visit the American Academy of Periodontology — a trusted source for evidence-based information on periodontal health.
Why Choose Arlington Dental for Your Gum Surgery?
Arlington residents can trust Arlington Dental for safe, compassionate periodontal care. Our dentists and periodontists have extensive experience treating gum disease, and we use the latest technology to make surgery efficient and comfortable. We offer sedation options and sedation dentistry for anxious patients to ensure you feel at ease. Our office at 43 Broadway, Arlington, MA (contact info below) is fully equipped for oral surgery and follows strict infection-control standards.
Most importantly, we take time to explain your diagnosis and options. Before suggesting surgery, we will exhaust all non-surgical treatments. If surgery is needed, we’ll walk you through each step, answer all your questions, and follow up closely. Patient trust and safety are our top priorities. Many patients have reported positive experiences — they appreciate that we make complex treatments “comfortable” and treat them with care.
If you have been diagnosed with moderate to severe periodontal disease, we invite you to schedule a consultation with our dental team. Early intervention is key: the longer gum disease is left untreated, the more extensive surgery may be. Let our Arlington Dental specialists help restore your gum health and protect your smile.
People Also Ask
What is osseous surgery and why is it done? Osseous surgery (also called pocket reduction surgery) is a periodontal procedure for advanced gum disease. It’s done when deep gum pockets harbor bacteria that cannot be cleaned by brushing or scaling. During the surgery, the gums are lifted to remove infection and the bone is reshaped. This reduces pocket depth and allows the gums to reattach more tightly to the teeth.
How do I know if I need osseous surgery? Your dentist may recommend osseous surgery if periodontal pocket depths remain 5 mm or deeper after non-surgical treatment, or if X-rays show jawbone defects. In practice, this means that if deep cleanings and antibiotics haven’t fully resolved your gum disease, a periodontist will suggest surgery.
Is osseous surgery painful? You should not feel pain during the procedure because local anesthesia (numbing) is used. Most patients report feeling only pressure while the dentist works. After surgery, you may experience mild soreness or swelling, but this is typically controlled with over-the-counter or prescribed pain medication. In general, it’s much less uncomfortable than many patients expect.
How long does recovery take after osseous surgery? Initial healing of the gums takes about 1–2 weeks. You can return to most normal activities (eating soft foods, gentle oral hygiene) within a few days to a week. Swelling and discomfort usually peak in the first 48 hours and then improve. The gums will fully stabilize in a few months, but you will see most of the improvement and resume a normal diet by 3–4 weeks.
Will I need bone grafting during osseous surgery? Sometimes. If a lot of bone has been lost from periodontal disease, your dentist may place bone graft material at the time of surgery to encourage new bone growth. This grafting helps rebuild lost support around the teeth. Your periodontist will let you know if grafting is recommended in your case.
How effective is osseous surgery at treating gum disease? Osseous surgery has a high success rate for controlling periodontitis. By removing infection and reshaping the bone, it drastically lowers pocket depths. When combined with good oral hygiene afterward, it greatly increases the chance of keeping your natural teeth long-term. Patients typically see healthier gums and far less bleeding after healing.
Are there alternatives to osseous surgery? For mild gum disease, yes – scaling and root planing (deep cleanings) can often suffice. Some laser-based therapies (like LANAP) may also help treat pockets without cutting. However, these are not a substitute in every case. When deep pockets remain, osseous surgery is considered the gold standard to fully access and clean the roots and bone.
How much does osseous surgery cost in Arlington, MA? Costs can vary depending on how many teeth and areas are involved. As a reference, Massachusetts fee schedules list around $700–$800 per quadrant of teeth, but actual charges depend on the dentist and your individual needs. Insurance often covers a portion of periodontal surgery – check your benefits. Arlington Dental will provide a personalized estimate after your exam.
How should I prepare for osseous surgery? Follow your dentist’s instructions. Generally, continue your regular medications unless told otherwise. You may be advised to stop blood thinners (like aspirin) a few days before. Eat a nutritious meal before the appointment, since you will be numb afterward. Avoid alcohol and smoking 24 hours before and after. Arrange a ride home if you choose sedation, as you won’t be able to drive immediately.
Can I have sedation during osseous surgery? Yes. While local anesthesia is standard (you’ll feel pressure but no pain), many offices offer sedation options. In Arlington, sedation dentistry (oral sedatives, nitrous oxide, or IV sedation) is available for anxious patients. You will remain comfortable and relaxed during the procedure, with the dental team monitoring you throughout.
Frequently Asked Questions
What exactly happens during osseous surgery?
Your periodontist will numb the area, make incisions to lift the gums, and thoroughly clean the exposed roots. Any diseased bone is smoothed (and grafted, if needed). The gums are then stitched back in place over the reshaped bone, creating shallower pockets.
How long does the osseous surgery procedure itself take?
The procedure typically takes 30–60 minutes per treated area (quadrant of the mouth). It depends on how many teeth need treatment. Your dentist will plan the timing based on your case.
Is osseous surgery covered by dental insurance?
Many dental insurance plans do cover periodontal surgeries like osseous surgery (often at 50% after the deductible). Coverage varies by plan, so we recommend checking your periodontal benefits. Arlington Dental’s staff can help verify your coverage and file claims.
What kind of anesthesia will be used?
Osseous surgery is usually done under local anesthesia (injections to numb the gums). You will feel no pain. For extra comfort, you can choose sedation (laughing gas or oral/IV sedation) so you remain very relaxed. We will discuss anesthesia options during your consultation.
Will I have stitches and what happens to them?
Yes, small sutures are placed to hold the gums in the new position. Many dentists use dissolvable stitches that disappear in about 1–2 weeks. If non-dissolvable sutures are used, a follow-up visit will be scheduled to remove them.
What foods can I eat after osseous surgery?
Stick to soft foods for the first few days. Examples include yogurt, soup (not too hot), applesauce, pudding, scrambled eggs, mashed potatoes, and smoothies. Avoid crunchy, hard, spicy or very hot foods that might irritate or injure the surgical site. Gradually return to your normal diet as the healing progresses.
How do I care for my mouth after surgery?
Keep the area clean with gentle rinsing and any prescribed antimicrobial mouthwash. Brush and floss the other teeth as usual. In the treated area, be very gentle around the stitches. Follow all of Arlington Dental’s post-op instructions closely. Good home care is essential for the surgery to succeed.
Will my gums grow back after osseous surgery?
No. Periodontal disease permanently destroys gum tissue. Osseous surgery stops further loss but does not replace missing gum. If gums recede and expose roots, a separate gum grafting procedure is needed to rebuild lost gum tissue.
What are the risks of osseous surgery?
Risks include infection, bleeding, postoperative sensitivity or slow healing. There is also a chance of increased gum recession around treated teeth. These are uncommon when proper care is taken. The dental team will give you detailed instructions to prevent complications. In general, the health benefits far outweigh these minimal risks.
How successful is osseous surgery long-term?
When combined with good oral hygiene and regular maintenance cleanings, osseous surgery is very successful at controlling gum disease. Studies show a high success rate in preserving teeth after surgery. Many patients maintain healthy gums for years afterward, significantly extending the life of their natural teeth.
Conclusion
Osseous surgery is a powerful, proven solution for managing advanced periodontal disease and preserving your natural teeth. While the idea of gum surgery may sound intimidating, modern techniques, expert care, and effective anesthesia make the procedure comfortable and routine for most patients. By eliminating harmful bacteria, reducing deep pockets, and restoring healthy bone contours, osseous surgery gives your gums the chance to heal — and your smile the support it needs to last a lifetime.
If you’ve been struggling with persistent gum issues or have been told you need periodontal treatment, don’t wait. The sooner you take action, the easier and more effective treatment will be. At Arlington Dental, our experienced team is here to guide you every step of the way with compassion, clarity, and outstanding care. Choose the best dentist in Arlington, MA. Visit Arlington Dental, 43 Broadway, Arlington, MA 02474. (781) 641-0500.